Men’s Mental Health Month: Plan in October, Make June Count
June is a pivotal moment to champion men’s emotional wellbeing and make support visible, practical, and inclusive. This announcement distills what matters most—what the month is, why it’s urgent, and exactly how to activate your workplace, campus, team, or community with minimal lift and maximum impact. Whether you’re an HR leader, educator, nonprofit organizer, coach, or faith-based volunteer, you’ll find plug-and-play tools to kickstart efforts that reduce stigma, normalize help-seeking, and connect men to care.
As you plan for men's mental health month, this guide offers employer-focused checklists, event timelines and budgets, ready-to-share social posts and email copy, and assets tailored to reach men across cultures and identities—including BIPOC and LGBTQ+ communities. You’ll also get up-to-date statistics to ground your messaging, plus clear referral pathways to helplines, NAMI chapters, and clinical resources.
Start here to turn awareness into action and ensure every man in your network knows support is real, reachable, and respected.
What is Men's Mental Health Month and when is it observed?

Men’s Mental Health Month is observed every June as a dedicated time to elevate men’s mental health awareness, reduce stigma, and connect men and boys with support. The focus is broad: preventing crises, encouraging early screening, and normalizing conversations across workplaces, schools, and community spaces.
While mental well-being is relevant year-round, a concentrated month helps organizers coordinate events, share consistent messages, and track impact. It also provides a timely hook for media, employers, and local coalitions to spotlight prevention, coping skills, and help-seeking. For families and partners, June is an opportunity to check in, share resources, and encourage care with empathy.
For clinicians and advocates, it’s a chance to reach men who might otherwise stay silent. Taken together, this annual observance creates momentum to support men’s mental health in practical, measurable ways.
Background and history of the month
Men’s mental health got a formal boost in the 1990s when momentum around preventable men’s health issues led to federal recognition. In 1994, National Men’s Health Week was established to highlight screenings and encourage early intervention. This observance, anchored in June, helped organizations and public health agencies formalize outreach that included—but wasn’t limited to—mental well-being.
“President Clinton signed the bill on May 31, 1994 thereby establishing National Men’s Health Week.” Men’s Health Month
Over time, many advocates and communities expanded the conversation beyond physical checkups to emotional health, stress, and suicide prevention. That shift reflects lived experience: men often delay care, downplay symptoms, or fear judgment for speaking up. A month-long frame gives space for practical education on warning signs, language to reduce stigma, and pathways to care. It also helps workplaces, schools, and faith communities align activities—like screening days, peer support launches, and storytelling campaigns—with a common theme and calendar.
Today, Men’s Health Month in June remains a unifying platform. It bridges physical and mental wellness, encourages inclusive messaging for diverse communities, and invites families to take action together. By spotlighting mental health alongside preventive care, June drives earlier conversations and stronger connections to help.
June vs. November (Movember): why both months matter
June and November both mobilize attention for men’s well-being—but they play different, complementary roles. June’s Men’s Health Month centers prevention and broad mental health awareness, inviting organizations to run screenings, host panels, and share resources. November’s Movember is a grassroots movement best known for mustache-led fundraising that focuses on prostate and testicular cancer, as well as men’s mental health and suicide prevention. Together, they create two touchpoints each year to keep conversations alive and services visible.
A quick look at how they compare:
- Timing: June (Men’s Health Month) vs. November (Movember)
- Primary mode: Education and community programming vs. fundraising plus peer-led campaigns
- Emphasis: Broad preventive care and mental health vs. specific cancers and suicide prevention (with mental health woven in)
- Ideal activations: Summer wellness fairs, workplace trainings, and screening drives vs. storytelling, peer challenges, and donation campaigns
“In 2024, 23.40% of adults in the U.S. experienced any mental illness (AMI) in the past year, equivalent to over 60 million people.” Mental Health America
That scale underscores why multiple moments matter. June can launch skills-building—like stress management and help-seeking—while November can reinforce peer support, fundraising for services, and suicide prevention messaging. For teams planning calendars, use June for learning and systems changes, and November to re-engage audiences with stories, challenges, and giving.
Key statistics and why awareness matters

Numbers illustrate both the urgency and the opportunity. Men experience mental health conditions at significant rates, yet many remain undiagnosed or untreated. Stigma, cultural expectations, and limited access to care can keep symptoms hidden until they become crises. June’s outreach helps normalize check-ins, screenings, and therapy—before emergencies arise.
“Mental health disorders affect 1 in 8 men globally, yet many go undiagnosed or untreated. Depression alone impacts over 6 million men in the U.S., with suicide ranking as the 7th leading cause of death among men.” Revive Research Institute
These men’s mental health statistics point to specific actions. First, education should highlight common signs—sleep changes, irritability, substance use—so partners and peers can spot concerns early. Second, campaigns should showcase diverse stories that reflect different ages, cultures, and identities, reducing the pressure to “tough it out.” Third, workplace and community leaders can make pathways to care visible and simple: anonymous screenings, EAP reminders, walk-in hours, and telehealth options. When men see care as practical, confidential, and goal-oriented, they are more likely to engage.
Micro-conclusion: June’s Men’s Mental Health Month clarifies what it is, why it exists, and how it complements November’s Movember to keep momentum year-round. With history as a foundation and data underscoring the stakes, the next step is practical action—see the upcoming section on workplace initiatives for men’s mental health to start planning. Don’t miss our event organizer toolkit to streamline your outreach.
How organizations, workplaces, and communities can observe
June is a natural on-ramp for action—whether you’re an employer, nonprofit, campus, or neighborhood council. The goal is to normalize help-seeking, reduce stigma, and create visible touchpoints that meet men where they are: at work, online, on teams, and in community spaces. A strong plan blends policy changes, training, and storytelling with simple, repeatable activities that any group can run. Thoughtful inclusion matters, too—design outreach with BIPOC and LGBTQ+ men in mind, and make sure materials reflect the people you want to reach. As you build, reference your culture and constraints, then prioritize quick wins you can sustain beyond men's mental health month.
Workplace initiatives: checkpoints, policies, and trainings
A credible workplace effort starts with leadership signaling support and making it easy to participate. Publish a short CEO/leader note, activate managers with talking points, and promote benefits in plain language. Then, pair culture cues with measurable steps: a 5–10 item pulse survey, EAP promotion with guaranteed confidentiality reminders, and a schedule of brief trainings. This approach sets expectations and builds momentum while respecting time and privacy.
"Organizations should engage in comprehensive mental health planning for the workforce. As they do with other important employee populations, employer plans should include strategies to meet the unique needs of male employees." WTW
- Checkpoints to run this month:
- Leadership pledge and visible participation in at least one event.
- Manager cascade: 10-minute huddle script, FAQs, and referral pathways.
- Benefits spotlight: EAP, therapy coverage, peer support, and self-guided tools.
- Privacy-first comms: clarify no data is shared back to managers.
- Inclusive visibility: images and examples reflecting diverse men and families.
- Policy tune-ups that signal care:
- Explicitly allow mental health as a reason for sick leave.
- Ensure parity in coverage for counseling, teletherapy, and medication.
- Add flexible scheduling for appointments and support groups.
- Partner with ERGs/unions to co-design programming and feedback loops.
- Trainings that fit busy schedules:
- “Recognize and Refer” micro-sessions for managers (15–30 minutes).
- Gatekeeper or psychological safety primers for team leads.
- Bystander skills to counter stigma and harmful banter.
- Male-focused support spaces: facilitated drop-ins or peer circles.
Track participation, anonymized EAP inquiries, and post-training confidence. Close the loop by sharing what you learned, adjusting supports, and committing to one sustained practice (for example, quarterly manager refreshers).
Event organizer playbook: timeline, budget, and checklist
A simple, time-bound plan keeps everyone aligned. Start with your goal (awareness, engagement, or referrals) and map actions backward from your event date. Build in inclusive outreach—partner with barbershops, community centers, veterans’ groups, faith communities, and LGBTQ+ orgs to reach men who may not see themselves in traditional messaging.
| Timeline | Key actions |
|---|---|
| T–8 weeks | Define goals and audience; confirm venue/date; recruit partners/speakers; draft budget and roles. |
| T–6 weeks | Secure vendors; finalize agenda; request marketing assets; begin outreach to community partners. |
| T–4 weeks | Launch save-the-date; open registration; confirm accessibility needs (ASL, captions, ramps, childcare). |
| T–2 weeks | Promote weekly on social and email; brief volunteers; order materials; confirm tech and livestream. |
| T–1 week | Send reminders; run tech check; prepare day-of run-of-show and escalation plan. |
| Event day | Execute run-of-show; welcome desk; feedback QR; quiet space available; list referrals. |
| T+1 week | Send thank-you + resources; review feedback; publish recap with next steps. |
- Budget categories:
- Venue/AV, captioning/translation, childcare, refreshments, speaker honoraria, design/printing, livestream, volunteer appreciation.
- Cost-savers: co-host with partners, use community spaces, digital-only toolkits, sponsor-donated refreshments.
- Checklist essentials:
- Registration form with pronouns and accessibility needs.
- Inclusive visuals and copy; content warnings where appropriate.
- Clear referral sheet for support and non-crisis resources.
- Feedback form with optional demographics to assess reach.
- Safety and de-escalation contacts; quiet room and water.
Document what worked, who you reached, and what to improve. Share a short recap with partners and invite them to co-create a fall or winter follow-up.
Resources, crisis support, and downloadable assets
When someone is ready to open up, having the right resource at the right moment matters. This section gathers practical, immediate options you can offer men, families, and colleagues—from crisis helplines and clinical referrals to community-based peer groups and a ready-to-use communications toolkit. Whether you’re a workplace lead, organizer, or community advocate, you’ll find centralized guidance to make conversations safer and next steps clearer during Men's Mental Health Month. Use this as your “save and share” hub throughout June and beyond, and adapt it for diverse audiences, including veterans, BIPOC and LGBTQ+ men, fathers, students, and older adults.
Helplines & clinical resources: where to refer
Start with crisis options first, then move to ongoing care. In the U.S., people can call or text 988 for immediate support if they’re in emotional distress or concerned about someone else. Outside of emergencies, encourage men to contact their primary care provider or a trusted clinic to discuss screenings, referrals, and potential medication management. If you have an Employee Assistance Program (EAP), promote confidential brief counseling and referral pathways. Telehealth platforms can reduce time and stigma barriers—highlight evening hours, chat-based therapy, and options for men who prefer text over video. For veterans, point to VA mental health services and peer support specialists; for college men, route through campus counseling with after-hours lines.
Quote and share one clear description of what confidential, nonjudgmental help looks like to make it feel approachable:
“The NAMI HelpLine is a free, confidential nationwide service that provides one-on-one emotional support, mental health information and resources needed to tackle tough challenges that you, your family or friends are facing.” NAMI
After the immediate step, outline next options in writing:
- Primary care visit for screening and referrals (PHQ-9, anxiety screens).
- Short-term counseling via EAP or telehealth; consider male-identifying or culturally responsive clinicians.
- Group therapy or skills programs (CBT, ACT, mindfulness) that fit schedules and privacy needs.
- Safety planning and means-safety resources if suicide risk is present.
Keep follow-up simple: offer to help make the first appointment, set reminders, and normalize trying a few therapists to find the right fit.
Local support: finding NAMI chapters & peer groups
Local connection can sustain recovery between clinical visits. Direct people to search for a nearby NAMI chapter using the organization’s locator; chapters often host free peer-led groups, family programs, and educational classes. Encourage men to check meeting formats (in-person vs. virtual), timing (evenings/weekends), and any identity-specific groups that increase comfort and relevance—such as groups for veterans, Black men, Latino men, or LGBTQ+ men. Community partners can also help: faith organizations, barbershops, cultural centers, fraternities, and recreation leagues often know trusted local supports.
Tips to evaluate and choose the right peer space:
- Confidentiality and ground rules are explained up front.
- Facilitators are trained peers or clinicians; meetings have a clear structure.
- Accessibility is addressed (location, cost-free options, language, transportation).
- Clear guidance for what to do between meetings and how to reach help if symptoms worsen.
If you’re organizing, consider co-hosting with community leaders men already trust. Offer practical draws—childcare, a meal, or a skills mini-workshop (sleep, stress, money management)—to reduce barriers to attendance. Promote consistency (same day/time), publish a seasonal schedule, and collect anonymous feedback to refine topics. Finally, help attendees map a personal support plan: who to call, where to go locally, and one skill they’ll practice this week.
Asa.Team: mental health support into everyday workflows
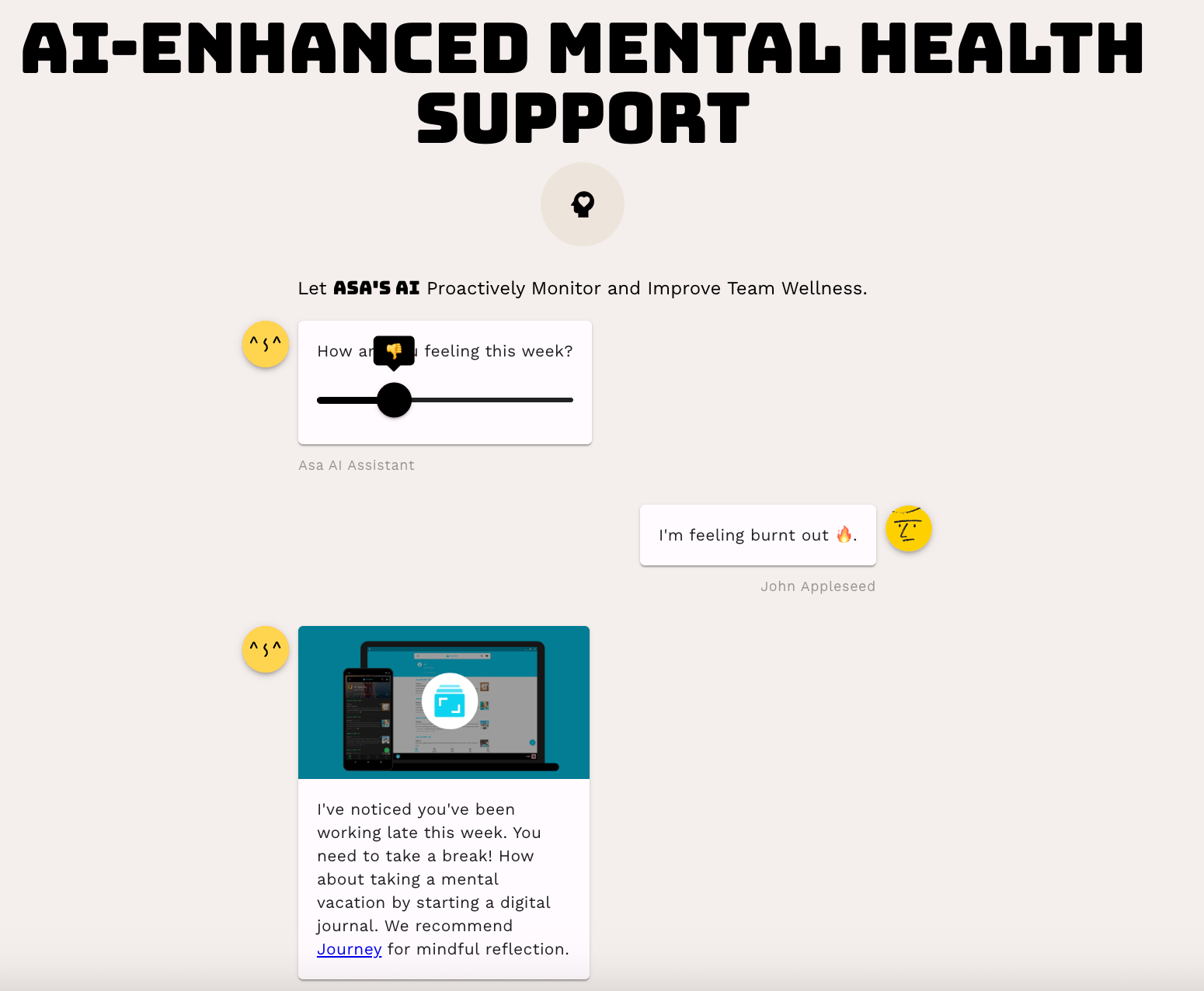
Asa.Team’s mental health layer is built to reduce stigma and make support feel routine at work. It uses privacy-first wellness monitoring to surface aggregate signals—like sustained overtime, missed breaks, or unusual inactivity—without exposing any one employee. Managers see trends and recommended actions, not individual health data.
Toolkit: flyers, social templates, and event checklists
Equip your team with ready-made assets so outreach can start today. Keep language plain, empathetic, and action-focused; pair every message with a next step (text, call, attend, book). Use images that reflect the diversity of men by age, race/ethnicity, body type, and gender expression, and include alt text for accessibility.
Suggested assets and how to use them:
| Asset | What to include | Use it for |
|---|---|---|
| One-page flyer | Theme, top 3 resources (crisis, local, workplace/EAP), QR code | Breakrooms, gyms, clinics, barbershops |
| Social square (1080x1080) | Short headline, single action, alt text | Instagram, LinkedIn, Facebook |
| Story/reel caption | 1 empathy line + 1 action + hashtag | Stories, short videos |
| Email template | Subject, 3 bullets, signpost to help | Employee/newsletter blasts |
| Event checklist | Timeline, roles, supplies, metrics | Organizers and volunteers |
Copy-and-paste starters:
- Email subject: “June: You’re not alone. Support is here.”
- Email body bullets:
- Confidential help is available today.
- Join our men’s support hour on [date/time].
- Prefer texting? We’ve included options that fit your style.
- Social headline: “Strong doesn’t mean silent.”
- CTA lines: “Talk to someone today.” “Bookmark your support plan.” “Share this with a friend.”
- Alt text example: “Smiling Black father and teen son walking in a park; text reads ‘Strong doesn’t mean silent—support is here.’”
Event essentials checklist:
- Confirm venue/date; request ASL or language interpretation if needed.
- Prepare a resource table: crisis info, local groups, EAP details, QR codes.
- Brief speakers on inclusive language; add content notes for sensitive topics.
- Track attendance and questions; follow up with a “Resources Recap” email.
- Measure outcomes: resource clicks, sign-ups, referrals, post-event survey.
With crisis lines, clinical pathways, local peer spaces, and plug-and-play assets, you’re ready to move from awareness to action.