Mental Breakdown Signs & Recovery: Complete Guide to Causes, Help & Treatment (2025)

If you’re worried you’re having a mental breakdown—or supporting someone who might be—this guide offers calm, step-by-step help when everything feels overwhelming. We’ll show you the clearest signs of a mental breakdown, what to do in the next 10 minutes, and when to seek emergency help.
You’ll get a concise self-assessment and a printable safety-plan template, plus exact scripts for calling a hotline or speaking to a loved one in crisis. We’ll also cover nervous breakdown symptoms versus burnout, panic attacks, and depression—so you can name what’s happening and choose the right next step.
Beyond immediate relief, you’ll learn how to recover from a mental breakdown with a practical, clinician-informed plan: crisis supports, a paced return-to-work template, and a relapse-prevention checklist. We’ll include workplace and legal accommodation tips, financial supports, and a comprehensive list of US and international crisis resources to get real help fast.
To start on solid ground, clarity matters. First, we’ll explain what a mental (nervous) breakdown is—and how it differs from panic, burnout, and depression—so you can act with confidence.
What a Mental (Nervous) Breakdown Is — How It Differs from Panic, Burnout, and Depression
When people say “mental breakdown,” they usually mean a period when stress and symptoms pile up so intensely that daily life stops working. It’s a lay term, but the experience is real: severe distress, impaired functioning, and often urgent need for support.
Because “nervous breakdown symptoms” overlap with several conditions, confusion is common. Clear language helps you recognize signs of a mental breakdown versus a panic attack, burnout, or a depressive episode, so you can take the right next step.
Below, you’ll find a quick, practical map. First, what clinicians actually mean; then a side-by-side comparison; and finally, common mental breakdown causes, risk factors, and triggers that raise vulnerability.
Why 'mental breakdown' isn't a formal diagnosis and common clinical equivalents
“Mental breakdown” isn’t listed in diagnostic manuals. It’s a nonclinical phrase people use to describe a mental health crisis where functioning has collapsed—missing work or school, withdrawing from others, or feeling unable to cope. As Mayo Clinic notes, the phrase typically points to an underlying condition that needs assessment and care, not a standalone diagnosis.
Clinically, a “breakdown” may align with several diagnoses. Common equivalents include a severe major depressive episode, panic disorder with frequent or unexpected attacks, generalized anxiety disorder in acute flare, adjustment disorder or acute stress reaction after a major life event, post‑traumatic stress disorder, or an exacerbation of bipolar disorder. In some cases, substance use, medication effects, sleep deprivation, or a primary psychotic disorder can precipitate similar crises.
Clinicians look at duration, severity, and impairment: how long symptoms have lasted, how intense they are, and how much they disrupt work, self‑care, and relationships. They also rule out medical contributors (for example, thyroid issues, infections, or medication side effects) and assess for safety risks.
Bottom line: the label is less important than getting the right help. Still, knowing the distinctions can guide your immediate decisions and conversations with a provider.
Direct comparisons: breakdown vs. panic attack, burnout, depressive episode (quick reference)
Use this quick reference to tell look‑alike conditions apart. It can help you describe your experience and identify next steps if you’re unsure whether you’re facing a mental breakdown, panic attack, burnout, or depression.
| Feature | Mental breakdown | Panic attack | Burnout | Depressive episode |
|---|---|---|---|---|
| Onset | Builds over days–weeks; can feel like “hitting a wall” | Sudden, peaks within minutes | Gradual, months of chronic stress | Gradual or subacute over weeks |
| Hallmark | Global overwhelm + impaired functioning | Intense fear, chest tightness, palpitations | Emotional exhaustion, cynicism, reduced efficacy | Persistent low mood or loss of interest |
| Duration | Prolonged crisis until support intervenes | Brief (minutes–hour), may recur | Ongoing until workload/conditions change | ≥2 weeks most days |
| Drivers | Stacked stressors + underlying condition | Fight/flight surge; misinterpreted body cues | Work/role stress exceeding resources | Biological, psychological, social factors |
| Body signs | Sleep/appetite shifts, fatigue, tension | Shortness of breath, trembling, dizziness | Fatigue, headaches, GI issues | Appetite/sleep changes, low energy |
| Function | Markedly impaired across domains | Between attacks, function may be normal | Mainly work‑related impairment | Impairment across life areas |
| Risk flags | Suicidal thoughts, psychosis, inability to care for self | Fear of dying/losing control during attack | Detachment, errors, accidents | Suicidal thoughts, marked slowing or agitation |
Quick cues:
- If distress is brief but explosive with racing heart and fear of dying, think panic attack.
- If exhaustion, cynicism, and reduced capacity are tied to chronic work stress, think burnout.
- If mood is persistently down with loss of interest and daily impairment, think depressive episode.
- If multiple systems feel collapsed at once, you can’t function, and stressors have stacked, “mental breakdown” describes the crisis—seek timely support.
Next, understand what increases your risk so you can spot mounting pressure earlier.
Key risk factors and common triggers

A mental breakdown rarely comes out of nowhere. It’s usually the end point of accumulating pressures plus vulnerabilities. Cleveland Clinic highlights contributors such as chronic work or caregiving stress, major life changes, trauma, financial/legal strain, sleep deprivation, and health issues; personal or family mental health history and substance use also raise risk.
Common triggers include:
- Acute stressors: job loss, breakup, bereavement, accidents, or public conflict.
- Chronic stressors: workload spikes, understaffing, discrimination, academic pressure, or ongoing caregiving demands.
- Biological factors: insomnia, chronic pain, thyroid or hormonal shifts, postpartum changes, and some medications or substances (including alcohol/stimulants).
- Social factors: isolation, lack of support, unstable housing, or unresolved conflict at home or work.
- Psychological factors: perfectionism, high self‑criticism, trauma history, or poor boundaries.
Risk isn’t destiny. Protective factors—regular sleep, supportive relationships, skills for emotion regulation, and reasonable workload—buffer stress. But when several triggers stack (for example, sleep loss + financial worry + conflict at work), vulnerability rises sharply.
Asa.Team recognizes that mental wellness is crucial for workplace productivity and employee satisfaction. We track team mood averages to give employers real-time insights into their workforce's wellbeing, enabling proactive intervention before burnout or mental health crises escalate.
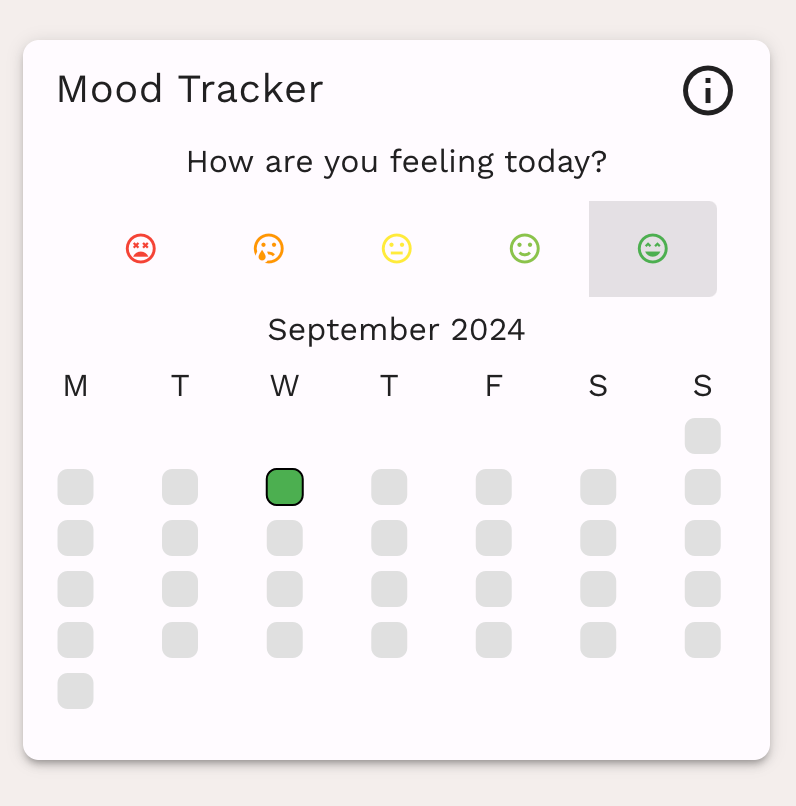
This data-driven approach helps create healthier work environments and supports timely mental health resources where they're most needed.
If you recognize mounting triggers plus worsening signs of a mental breakdown, plan proactive support now; earlier action often prevents a full‑blown crisis.
Recognizing Signs of a Mental Breakdown, Red Flags, and Immediate Actions

You now know a “mental breakdown” is a severe, time-limited mental health crisis rather than a formal diagnosis. Building on those distinctions from panic, burnout, and depression, this section focuses on what to notice right away and what to do in the next hour. You’ll find a concise checklist of nervous breakdown symptoms you can print or copy, clear red flags that signal when to seek emergency help, and a minute-by-minute set of grounding steps to stabilize.
Think of this as crisis-first aid. The goal is not to label yourself, but to quickly assess safety and functioning, then take the smallest next effective step. If multiple signs of a mental breakdown cluster at once and you can’t get through essential tasks, treat it as a mental health crisis and follow the red-flag guidance below. Keep this page handy; the scripts and checklists are designed to be used in the moment.
Core emotional, cognitive, behavioral, and physical symptoms (concise checklist)
Below is a concise, printable self-checklist of signs of a mental breakdown. Check what’s true today or this week; multiple checks across categories signal an urgent need for support.
- Emotional
- Overwhelming anxiety, dread, or fear that doesn’t ease
- Irritability or sudden anger spikes; tearfulness or emotional numbness
- Hopelessness, feeling “broken,” or persistent guilt/shame
- Cognitive
- Racing or looping thoughts; constant catastrophizing
- Concentration collapse, decision paralysis, or memory lapses
- Feeling detached or unreal (dissociation)
- Behavioral
- Withdrawing from people; skipping work/school or essential tasks
- Sleep extremes (almost none or sleeping all day) or neglecting self-care
- Sudden increase in alcohol/drug use or other impulsive behaviors
- Physical
- Chest tightness, shortness of breath, trembling, or dizziness
- Headaches, stomach upset, nausea, or appetite changes
- Exhaustion that rest doesn’t fix; sweating or chills
Quick self-assessment
- If you check several items across at least two categories for most of the day over 2+ days, or you can’t perform basics (eat, hydrate, sleep, show up), treat this as a mental health crisis and seek help now.
- If any items include thoughts about harming yourself or others, see the red flags section next and escalate immediately.
Red flags that require emergency help and exact scripts for calling/triaging
Escalate to emergency or urgent care if any of the following are present:
- Thoughts, plans, or intent to harm yourself or someone else
- Inability to care for basic needs (can’t maintain safety, hydration, or shelter)
- Severe confusion, disorientation, or hallucinations
- Sudden, extreme agitation; you feel out of control
- Severe substance intoxication/withdrawal or mixing substances with meds
- Chest pain, fainting, seizures, or other acute medical symptoms
According to guidance from the U.S. Department of Health and Human Services, recognizing intense stress and reaching out promptly is critical; see MentalHealth.gov for crisis tips and resources.
Use these exact scripts
- Key triage details to provide:
- Exact location and callback number
- Current risks, substances or meds involved, and medical symptoms
- Triggers, de-escalation tips, and language/access needs
- Pets or hazards on scene
If you’re helping someone:
“I’m calling about a mental health crisis for [Name, if known]. We’re at [Location]. Current risk: [suicidal thoughts/violence risk/disorientation]. They [do/do not] have access to weapons. Please send crisis-trained responders.”
If you’re the person in crisis:
“I need mental health crisis help. My name is [Name]. I’m at [Location]. I’m having [suicidal thoughts/no plan but can’t stay safe/severe panic/can’t care for myself]. I have [medical conditions/medications, if any]. I need help to stay safe.”
In the U.S., call 988 for the Suicide & Crisis Lifeline. If imminent danger, call 911 and request crisis-trained responders. Outside the U.S., call your local emergency number or nearest hospital.
Practical minute-by-minute steps and grounding techniques to use now
Use this 15-minute plan to reduce intensity and regain control. If symptoms worsen or safety is uncertain, escalate using the scripts above.
Minutes 0–2: Orient and slow down
- Say out loud: “I am safe enough in this moment. This will pass.” Name three true facts (date, place, one object you see).
- Exhale slightly longer than you inhale for 6 cycles. Drop your shoulders; unclench your jaw.
Minutes 2–5: Ground the senses
- 5-4-3-2-1: Name 5 things you can see, 4 feel, 3 hear, 2 smell, 1 taste.
- Hold something textured or cool (ice, a cold can) and describe it for 30 seconds.
Minutes 5–10: Regulate the body
- Box breathing: Inhale 4, hold 4, exhale 4, hold 4 (repeat 4 times).
- Progressive release: Tense and relax major muscle groups from feet to face.
- Sip water; avoid caffeine/alcohol right now.
Minutes 10–15: Reconnect and choose the next small action
- Text or tell someone: “Having a tough wave. Not in danger. Can you check in for 10 minutes?”
- Pick one 5-minute task: shower, step outside, or eat a small snack.
- Set a 30–60 minute re-check timer and decide your next step (call a trusted person, schedule urgent care, or use crisis services).
For a fuller menu of grounding options you can rotate through—physical, mental, and sensory—see this practical roundup by Healthline. Keep a short list of your top three techniques on your phone’s lock screen so you can use them quickly during a mental health crisis.
Treatment, Recovery Plan, and Prevention — A Practical Toolkit for a Mental Breakdown
You’ve learned what a mental (nervous) breakdown is and how it differs from panic, burnout, and depression. You’ve also reviewed urgent signs and immediate grounding steps. This final section turns insight into action: a step-by-step playbook to access clinical care fast, stabilize, and rebuild your life with guardrails against relapse.
We’ll start with short‑term supports and crisis services, then move into a copy‑and‑paste recovery template that includes a safety plan, a paced return‑to‑work approach, and a relapse‑prevention blueprint. Finally, you’ll find guidance on workplace/legal protections, building social supports, and a concise list of US + international hotlines for mental health crisis help.
The goal is practical: reduce risk today, make clear choices this week, and set up sustainable supports for 2025 and beyond. Keep this section handy—print it, share it with a trusted person, and use it as your recovery roadmap.
Short-term supports and clinical options (crisis services, meds, urgent therapy) with next-step checklist
If you’re in crisis now: call or text 988 in the U.S. for the Suicide & Crisis Lifeline, or use the hotlines below for your country. Ask for a welfare check or mobile crisis if you can’t travel safely. Crisis stabilization units, urgent care clinics with behavioral health, and emergency departments can provide same‑day evaluations, safety planning, and medication starts.
Urgent clinical options to ask about:
- Crisis services: mobile crisis teams, crisis stabilization units, partial hospitalization (PHP), or intensive outpatient programs (IOP).
- Medications: short‑term options for sleep/anxiety; longer‑term antidepressants or mood stabilizers when indicated. Discuss risks, benefits, and follow‑up.
- Rapid therapy access: single‑session or bridge therapy, telehealth CBT/DBT skills, and safety planning.
- Care coordination: primary care + psychiatry + therapy; consider peer support and family sessions.
Evidence‑based treatments and service types are summarized by the National Alliance on Mental Illness in Treatment & Services (https://www.nami.org/About-Mental-Illness/Treatments).
Next‑step checklist (48–72 hours):
- Contact a crisis line for triage; document the plan.
- Book first available psychiatry/therapy; ask for waitlist + cancellations.
- Ask your clinician about PHP/IOP if functioning is impaired.
- Secure sleep: consistent schedule; discuss short‑term sleep meds if needed.
- Identify one supporter who can check in daily this week.
- Remove or lock away lethal means; set up a written safety plan (see below).
- Schedule a 1–2 week follow‑up before you leave any visit.
3-step recovery template: safety plan, pacing/return-to-work plan, relapse-prevention plan
Use the following templates as a copy‑and‑paste starting point. Keep them visible, share with your clinician and one trusted person.
Safety Plan (fill in now)
- My warning signs: …
- Internal coping (10–15 min each): …
- People/places that help me feel safer: …
- Professionals I can contact (names, numbers): …
- Crisis resources (country-specific): …
- Means safety (how I will reduce access to lethal means): …
Pacing & Return‑to‑Work (RTW) Plan
- Phase 1 (Stabilize, 1–2 weeks): limit workload to essential tasks; 2–3 hours of focused work/day; daily check‑in with manager; protected sleep and meals; no after‑hours email.
- Phase 2 (Build, 2–4 weeks): 60–80% hours; pre‑planned breaks; one challenging task/day; weekly therapy; one day remote if helpful.
- Phase 3 (Sustain, 4+ weeks): full duties with accommodations as needed; monthly wellness review; boundaries for meetings/notifications.
Relapse‑Prevention Plan
- Early warning signs for me: …
- My top 5 buffers (sleep, activity, connection, therapy skills, medication adherence): …
- Weekly maintenance habits (days/times): …
- If symptoms spike (24–48h plan): who I’ll tell, what I’ll pause, which skills I’ll use.
- Review dates (every 30–60 days) and who will review with me.
These templates make “how to recover from a mental breakdown” concrete and trackable.
Long-term resilience: workplace/legal considerations, social supports, and where to find help (US + international hotlines)
Work and school can become stabilizers when calibrated correctly. Under U.S. law, many people qualify for reasonable accommodations (flexible scheduling, reduced distractions, modified deadlines, remote work days). The Job Accommodation Network offers practical ideas and how‑to guidance for requesting and documenting accommodations for mental health conditions (https://askjan.org/disabilities/Mental-Health-Conditions.cfm). Tip: focus your request on functional needs (concentration, stamina, attendance), not diagnoses. Explore FMLA, short‑term disability, or medical leave for additional protection.
Strengthen social supports:
- Identify 2–3 allies (friend, family, peer group) and set regular check‑ins.
- Join a peer support or skills group (CBT/DBT) to maintain momentum.
- Build a relapse “early alert” system—give supporters permission to speak up if they see warning signs.
Crisis resources (save now):
- United States: Call/text 988; chat via 988lifeline.org. Veterans press 1; Spanish press 2.
- Crisis Text Line: Text 741741 (US), 686868 (Canada), 85258 (UK), 50808 (Ireland).
- United Kingdom: Samaritans 116 123; jo@samaritans.org.
- Australia: Lifeline 13 11 14.
- New Zealand: Call/text 1737.
- India: Kiran 1800-599-0019.
If your country isn’t listed, call your local emergency number or your health ministry’s mental health page.
As you look ahead to 2025, blend accommodations, peer/community support, and ongoing care. Review your plan quarterly and update after any life change.
Conclusion
A mental breakdown can feel overwhelming, but it is manageable with a clear plan. You learned what it is—and isn’t—how it differs from panic, burnout, and depression; you reviewed core signs and red flags that demand emergency help; and you now have a practical toolkit to stabilize, recover, and prevent relapse.
Next steps you can take today:
- Copy the safety plan above and fill it out; share it with one trusted person.
- Contact a crisis line or book an urgent clinical visit; ask about PHP/IOP if daily functioning is impaired.
- Set up a 2‑week calendar: sleep anchors, therapy/med check, one social connection, and brief daily movement.
- Draft a simple return‑to‑work request focused on functional needs and boundaries.
- Schedule a 30‑day plan review to update your relapse‑prevention steps.
Looking forward, expect faster access to teletherapy, same‑day crisis support, and stronger workplace mental health policies in 2025. Pair these evolving resources with your personalized safety, pacing, and prevention plans for durable progress.
You don’t have to navigate this alone. Reach out for mental health crisis help now, then use this roadmap to guide how to recover from a mental breakdown—one small, steady step at a time.